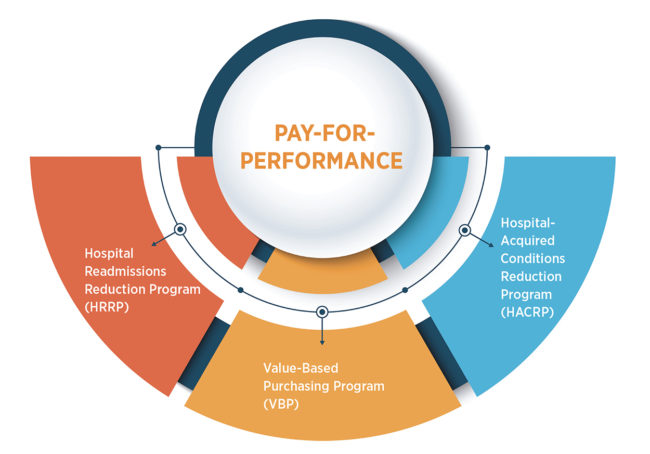
CMS pay-for-performance targets for hospitals
The Centers for Medicare & Medicaid Services (CMS) imposes financial penalties to hospitals that do not meet the standards for quality of care. The pay-for-performance (PFP) programs include:
- Hospital Readmissions Reduction Program (HRRP)
- Value-Based Purchasing Program (VBP)
- Hospital-Acquired Conditions Reduction Program (HACRP)
The three-part aim of the CMS PFP programs1
- Better care for individuals
- Better health for populations
- Lower costs
Cost to the system
In 2020, hospitals that fell short of meeting these standards received penalties from CMS, with these national results:
- Total pay-for-performance impact: $942 million
- HRRP impact: $550 million
- VBP impact: $823K
- HACRP impact: $391 million
Common traits2
Research shows those who are successful in these models have some things in common:
- Data-driven decision-making
- Care variability reduction
- Patient optimization
- Care transitions
- Physician engagement
- Cost reduction
Success in the New Reality
For the foreseeable future, PFP programs are here to stay. To be successful in this new reality, providers must ensure quality, cost-efficient care. To learn more, access CMS resources, including the toolkit referenced in footnote 2. For guidance on implementing or optimizing a service line structure within your organization, contact Kimberly Wright, RN, AVP of Clinical Services, at kimberly.wright@healthtrustpg.com
Sources:
- cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs
- innovation.cms.gov/files/x/bpci-toolkit.pdf





